By Larry Smith
It’s been a long time since we posted a blog. I’ve tried to write many times in the last year, but the words either just wouldn’t come, or the writing seemed too contrived, or it just seemed like garbage when I would read it back to myself. But I have decided that I have to write, even if it falls short of my expectations.
What a year and a half it has been! Going all the way back to February of 2020, life has been different.
Carol and I have learned so much about ourselves. And I have gained a new perspective on life and spirituality. We have both been changed by what we have gone through, hardened in some ways and softened in other ways.
This blog is necessarily going to be longer than the others. I need to tell our story first and then try to tell you what I have learned and how I have changed. So my plan is to split this into at least two parts.
I hope that you won’t find this to be boring. At best, I hope you can overlook the limitations of my writing ability and get a sense of what things are like for us now as you relive the last couple of years with Carol and me.
Where can I begin?
By late 2018, the strain of keeping an eye on my mother, who was beginning to show obvious signs of dementia, began to take a toll on Carol and I. Mother was still living by herself, but we had to keep a close watch on her to make sure she was okay.
Then she had two strokes, and the doctors said she could never live by herself again. She was in rehab, recovering from the strokes, when the pandemic hit in early 2020. Visitation was stopped at the rehab, and we weren’t able to see her.


When she was released in late March, 2020, I picked her up. The discharge nurse asked me to wait in the car, and I watched as two heavily gowned, masked, attendants wheeled her out.
A stay at home order had just been issued, and there were hardly any cars on the road as we made our way home. Most stores were closed, and there was an eerie silence all around us.
Though her dementia was worse, my mother noticed that we weren’t heading in the direction of her house, and I made the excuse that her doctors needed for her to stay with us for a while to make sure she was recovered.
Having mother stay with us totally interrupted our routines. But we knew it was in her best interest, and we were glad to try and make the best of it.
Actually, the pandemic had already interrupted all of our routines, especially my work one. Masks had begun to be required, and visitors into our buildings were severely limited. We bought point and shoot thermometers to take temperatures of all who entered buildings. Finally, the requirement to work at our offices was amended, and many employees began working from home.
A lot of visitors, and some employees, didn’t really take the pandemic seriously and barely took any precautions in our buildings. Mixed emotions and fear began to gradually increase as more and more people contracted the coronavirus.
My brother, Steven, who lives in Tennessee, reached out to me, asking if he could come down and live at my mother’s house while his apartment was being remodeled. It would take six months to a year for the apartment remodeling to be complete, and mother could go back to live in her home with Steven as the caregiver.

We felt that this was a good move for everyone, and it would help keep my mother safe from exposure to the virus. Although Carol and I tried our best to take precautions at home and work, we never felt totally safe because both of us worked around a lot of people. Mother and Steven would be isolated there at her home, and chances of them being exposed were minimal.
It turned out to be a good decision. On the third week of August, 2020, I developed a slight cough and a sore throat. Following protocol, I took off from work and went to get rapid-tested for the virus. Two hours later, the clinic called me, and I got the news that I didn’t want to hear. “Mr. Smith, you are positive for the corona virus.” Although my symptoms were mild, the clinic prescribed several medications for me.
I immediately called my doctor. His advice was to take the medications, keep an eye on my symptoms and hope for the best. I was his first covid patient, and he admitted that he didn’t really know how to treat the virus.

The night after my positive test results, I even got a call from the Alabama Department of Public health asking for information about my covid experience. I was also asked to give the names and phone numbers of anyone I might have exposed to the virus.
My symptoms began to progress a little with a low-grade fever, headaches and loss of sense of taste being added. About two weeks after testing positive, the symptoms were still fairly mild and I seemed to be getting better.
But then, at the beginning of the third week, I began to be plagued with a strange and devastating fatigue that literally knocked me down. Even with plenty of rest, I could barely even walk across the room without becoming totally exhausted. I would get up in the morning feeling fairly energetic, and fifteen minutes later I would have to go somewhere and sit down because I was so weak and dizzy. Also, my cough worsened, affecting my ability to sleep.
We called my doctor, and he said I needed to get to the emergency room at a nearby hospital as soon as possible. Carol said she could take me, and we started getting ready immediately.
I decided to take a shower before going, and that’s when I realized for the first time that something was bad wrong. While in the shower, I became extremely dizzy and felt as if I was going to pass out. When I tried to step out of the shower I barely had the energy to take the step and almost fell. I hadn’t noticed before but my breathing was shallow, and I felt very short of breath.
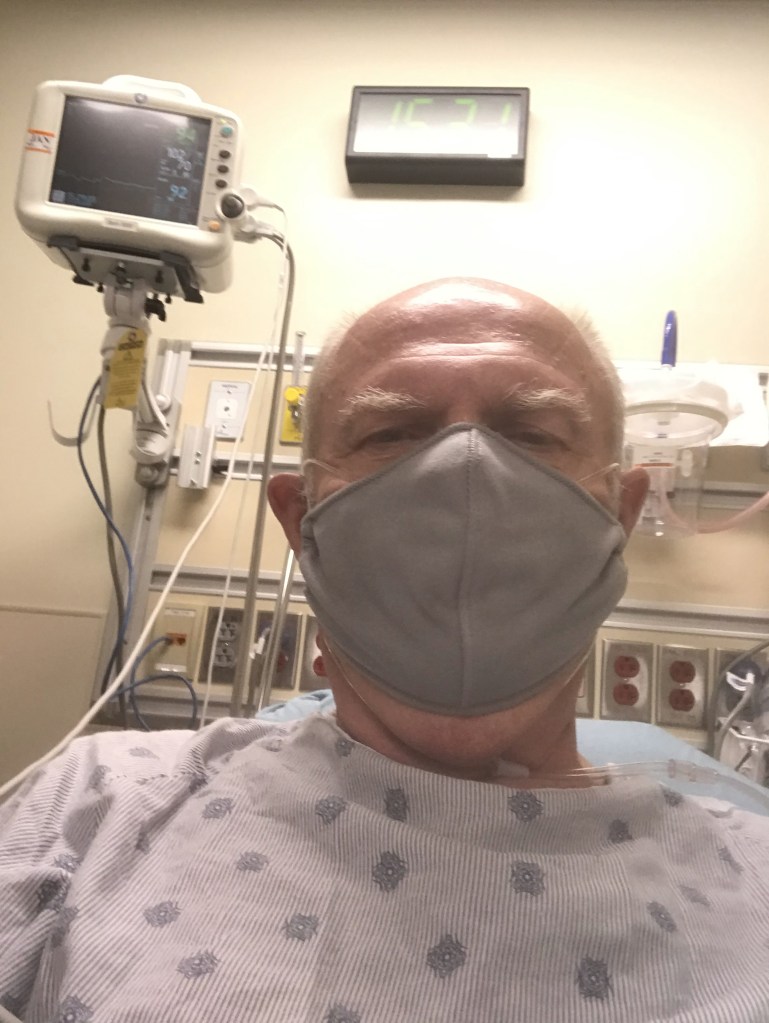
An hour later I found myself in a crowded emergency room full of masked people. Because I had covid symptoms, the ER staff prioritized my position on the examination list, and I was taken to a small room. A nurse put an oximeter on my finger to check my blood oxygen level. It was dangerously low, so she immediately applied supplemental oxygen. I was taken for several tests and then brought back to the exam room to wait for the results.
An hour later, the nurse came in to tell me that I had covid pneumonia in both lungs and was being admitted to the hospital. I texted Carol who was waiting in the car because no visitors were allowed in the hospital. “I’ll probably just be here overnight,” I said to reassure her.
Two hours later I found myself being wheeled through dark corridors to the floor where covid patients were housed. The entrances to the covid floor were covered with big squares of plastic, and it felt like we were going through the door flap of a tent. Once inside, I was taken through a noisy hall that was echoing with the sound of powerful exhaust fans.
In the room, a respirational therapist switched me over to a different source of oxygen. When my blood oxygen level failed to come up to a safe level, I was put on a more high-powered supplemental oxygen machine called the vapotherm. The force of the oxygen flow into my nose was strong and uncomfortable. And the hiss of the machine was loud and distracting.
Carol went back home without me. We are together all the time, and this was difficult for us. We made a vow to talk and text as much as possible and to try and figure out ways to carry on with our regular routine.
Alone in the semi-darkness of my room, I sat up on the edge of the bed. Attempting to stand up, I found that because of all of the tubes and wires that were connected to me it was just barely possible. From a standing position at the edge of my bed, I could not move at all to the right or left and could only move about three feet straight forward.
Morning came and my cough continued to get worse. The doctors tried several medicines, but nothing made it better. I was coughing constantly. Laying down made it worse, so I sat up all the time. Sleeping was out of the question, and as I became more and more exhausted, I also became more and more stressed out and agitated.
The constant noise of the oxygen machine, paired with the noise of the exhaust fans in the hallway, were driving me crazy. I complained to the nurses who said nothing could be done about it. One of the doctors prescribed Xanax for me, but I refused to take it.
Early evening of the third day, I took a turn for the worst and began struggling to breath. I pressed the call button and two nurses rushed to my side. Nothing they tried was helping, so they called the respiratory therapist. The blood oxygen level reading from my oximeter showed my percentage of O2 to be in the high 80s, but the therapist didn’t trust it. To get an accurate, real-time, O2 reading they drew blood from the tiny arteries in my wrist. It was extremely painful and took several tries before they could get the blood. An analysis of the blood showed that my actual blood oxygen level was 57 percent.
I was in big trouble. It is horrible to not be able to breath. I cried out to God for help, but all I sensed was darkness and emptiness. My life was out of my own hands. There was nothing I could do. I felt as if I was on the brink of passing out.
The respiratory therapist left the room and came back in with a huge machine. She said “we are going try the bipap.” A mask was placed on my face and pulled so tight that hardly any air couldn’t get in. “Just relax, the therapist said. Don’t try to breath on your own. Let the bipap breath for you.”

She turned on the big machine, and I immediately felt a strong suction pull all of the air out of my lungs. It was so powerful that it felt as if my lungs were deflating. Then just as quickly, oxygen was blown into my lungs causing the feel of my lungs being inflated. I tried to breath on my own but I was fighting a losing battle. I had to trust the therapist and the bipap.
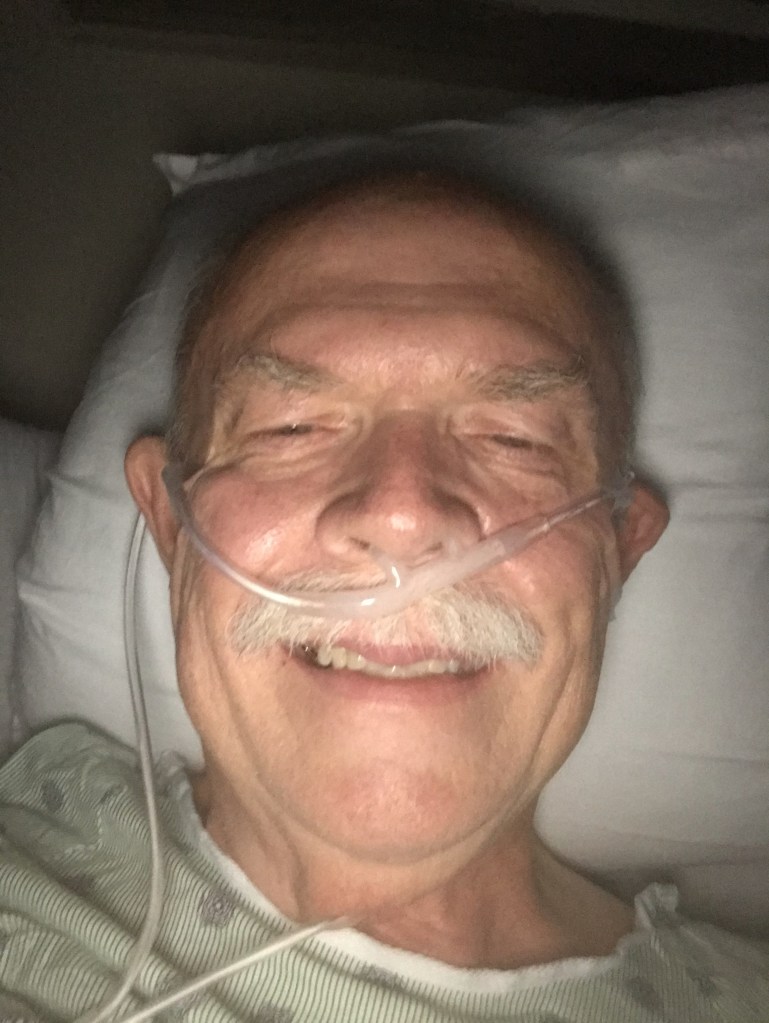
Making an effort to relax, I stopped consciously trying to breath and succumbed to the machine. It had a rhythm of its own and though it was very scary and uncomfortable, after a while I became accustomed to it. Strangely, I no longer felt that I was suffocating. The bipap was doing its job, and my oxygen level quickly climbed back up into the 90s on the display near my bed. Still not certain what was going to happen to me, I took a quick video on my phone of the bipap breathing for me and sent in in a text to Carol. Because my breathing was no longer being initiated by me, my cough stopped. For the first time in a couple of days I drifted off into a fairly deep sleep for a few hours.
Upon waking, however, I again became frightened by the suction of the machine when it pulled the air out of my lungs, I feared my lungs would collapse. I pressed the button to call the nurses station. When a nurse arrived, I first asked for a drink of water. The nurse said: “no I can’t remove your mask in order to give you a drink.” So I pulled the mask off myself and demanded the water.
The nurse called the respiratory therapist who hurried to my room and tried to make me put the mask back on. She said that if I didn’t continue to wear the bipap I would probably get worse and end up on a ventilator. I begged her to hook me up to the high powered oxygen again and see what happened. She finally gave in. Thankfully, back on the vapotherm, my blood oxygen level remained stable. The therapist said she would leave the bipap in my room just in case I took a turn for the worst.
My cough returned, and once again the sleep would not come. In addition, I developed nose bleeds caused by the constant flow of oxygen through my sinuses.
Carol and I texted and talked on the phone as much as possible. We read the bible together every night, prayed and made plans for what we wanted to do when I got well. Our talks and the scripture reading meant everything to me in that place of seeming darkness. I also got many much appreciated calls and texts from friends who prayed with me, read passages of scripture to me and just talked.
The doctors and therapists worked toward weaning me off the high-powered oxygen, but I wasn’t responding very well to the treatment. Every time they would try to lower the amount of supplemental oxygen I was getting, my blood oxygen would drop too low, and my heart rate would go up.
One day I had a real scare when my heart rate went over 200 bpm. A doctor prescribed a heart rate medicine for me. The first dose was given to me late one evening. A few hours later, I began to feel very weak. Looking at the heart rate monitor, I saw that my heart rate had gone way too low, almost down to 30 bpm. A nurse gave me something to bring the rate back up, and the next day I refused to take the heart rate medicine again. One of the doctors came by and convinced me to continue taking it but at only half of the original dose.
The days seemed to pass slowly, and I began to wonder if I was ever going to go home. I begged and badgered the doctors trying to make them send me home. I argued that being in the hospital was making me weaker rather than stronger. I threatened to get up and walk out on my own if they wouldn’t discharge me.
The problem was that my blood oxygen level, even with supplemental oxygen, was not stable. It seemed to have a mind of its own. When the therapists would try to reduce my supplemental oxygen level, my body would at first respond favorably with by blood oxygen level remaining in the 90s as long as there was only light movement or activity. But then, for no apparent reason, the O2 level would drop, and the supplemental oxygen level would have to be increased again. Though I campaigned for my doctors to discharge me and let home healthcare monitor this issue from my home, the doctors said no. They were afraid the O2 would drop too low unexpectantly and cause me to sustain organ damage or even die.
I was super frustrated and getting very impatient. I still felt that if I was home, with my wife and family, my stress level would be greatly reduced and healing would happen more quickly. Again and again I talked with the therapists and doctors asking to be discharged and threatening to walk out if they wouldn’t let me go. One of the therapists, who I had taken a liking to, told me that I had to stick it out in the hospital. He said that other COVID patients had walked out early, and almost every one of them had relapsed and had to be hospitalized again. He said every one of them had ended up on a ventilator and some had died.
Though the therapist’s warning scared me, I was equally as frightened because I wasn’t improving quickly, even with all the equipment and medicine the hospital offered. Even more than dying, I feared becoming weak and sickly and permanently disabled.
The hospital performed a barrage of tests on me trying to rule out the thyroid problems, heart problems, lung disease and other illnesses that my bloodwork and vital signs predicted.
Even with the treatment and therapy the hospital was giving, my breathing and blood oxygen levels were still impaired. Would I be sentenced by the virus to permanently require supplemental oxygen? Even with the heart rate medicine, my heart rate was unstable, jumping back and forth from 80 to 170 beats per minute as if it had a mind of its own.
I prayed as much as my lack of energy would allow. But I rarely prayed for myself. I prayed for Carol and for others in my family to be okay without me being there to do the things I had been doing for them.
Somewhere around the end of my second week in the hospital, my blood oxygen levels became more stable, and I was switched from the high powered oxygen to regular supplemental oxygen at a flow rate of 5 liters per minute. It still didn’t take much activity to make my O2 levels drop dangerously low. But the regular oxygen equipment was much quieter, and I was able to relax a little. My main doctor said that if I could get weaned down to 4 liters per minute, with O2 level not dropping below 88 percent when active, I could go home.
On the 18th morning of my hospitalization, the doctor signed my release order. Late that afternoon, Carol picked me up.
Though I barely had the energy, I packed up my belongings. I tried my best to hide my extreme fatigue from the nurses, fearing they would not release me if they knew.
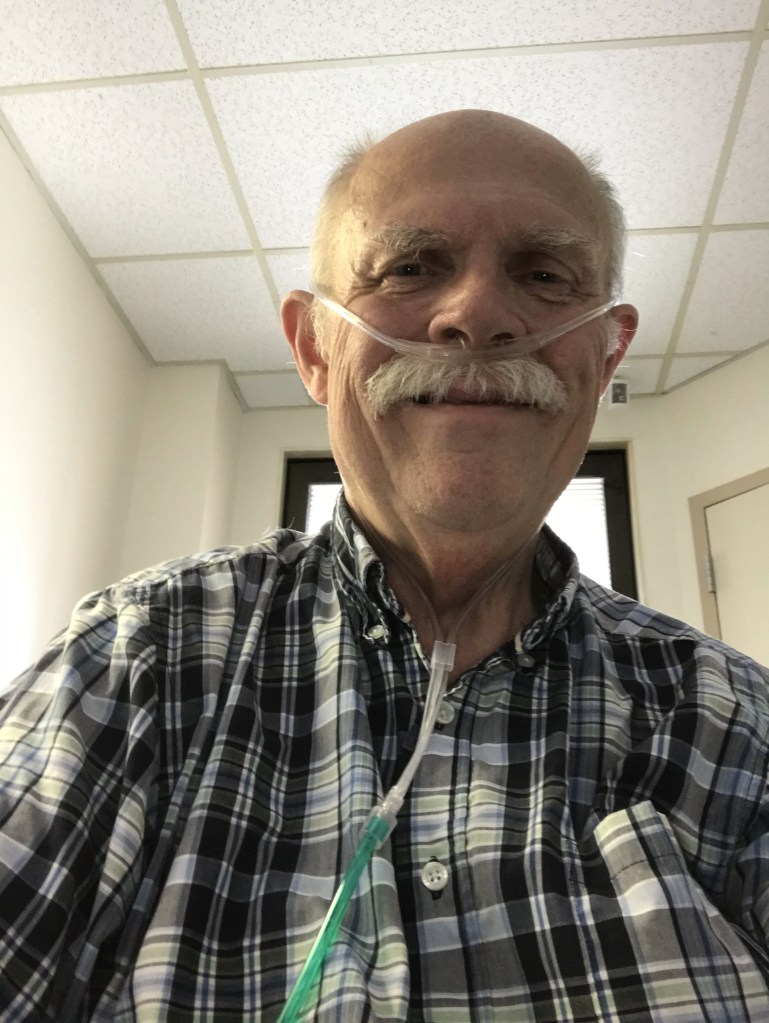
With oxygen tank trailing alongside me, I was wheeled out of the room, down the dark hall, into the elevator, out into the lobby where for the first time in almost a month I saw full sunlight.
Carol and the nurses helped me into the car. The sun was shining beautifully. For that matter, everything looked beautiful to me. It was as if I was seeing everything around me for the first time. The trees, the grass, the sky and even the cars and buildings looked new and wonderful.
I sucked in the oxygen from the little tank and prayed that I would be able to get home without getting too short of breath or experiencing a drop in my blood oxygen level. It felt so good to be free, and yet in the back of my mind I feared that something would happen to put me back in the hospital. I could tell that I was far from being well yet but tried my best not to show it.
About an hour after leaving the hospital, we pulled into the driveway of our home. I was never so glad to see that familiar porch and yard.
Stepping out of the car, I discovered that I was still too weak to walk. Carol suggested that I use the walker that had been prescribed for my mother a year before and went to retrieve it. Walking from the car to the house left me extremely winded, so I made a bee line for the recliner in the living room.
The medical equipment company had already been there and installed an oxygen concentrator. So I switched from the little tank to the concentrator. The concentrator had about 50 feet of hose attached to it, giving me the ability to walk from the living room to the bedroom, bathroom, kitchen and other parts of the house.Making my way to the back door I looked out on the patio. It seemed like a little piece of heaven to me.


My cough was still so bad that I couldn’t sleep lying down, so I opted to sleep in the recliner with Carol sleeping on the couch nearby.
A few days after getting out of the hospital I started physical and occupational therapy at home. I still felt weak, had breathing problems, was experiencing a high heart rate and coughing my head off. The brain fog from COVID was very bad, impaired my memory horrible and left me in a seemingly perpetual state of confusion. I felt dizzy most of the time and was unable to drive. I was glad to have the therapists. I wasn’t sure if I would ever get well, or if anyone could help me feel better, but at least, with the therapy, someone was keeping an eye on me, and I had a sounding board to express my concerns to.
With the therapy, I slowly began to get stronger, and my body began to do its job again. It took over three months for me to get off of supplemental oxygen during the day and have a safer, more stable heart rate. At the advice of my pulmonologist, I was still using oxygen when sleeping. I was to do so until I could be tested to see if my O2 level was safe during sleep.

The therapy had helped me tremendously. When the day came for me to be discharged I was apprehensive and skeptical about being without the support the therapy offered.
Though a lot better, I still had significant issues. There were still days when I felt short of breath, and my heart rate was still unpredictable, sometimes jumping as high as 170. I still had a severe cough and unexplained fatigue.
I continued going to a couple of different doctors, but neither of them offered a firm diagnosis or treatment. The bloodwork and tests I had didn’t yield definite answers.
Needing to return to some kind of normalcy, Carol and I moved out of the living room and started sleeping in the bedroom again. My cough was much worse when laying down, so I started out sleeping propped up in bed and slowly worked my way down to a laying position.
Slowly I started venturing out more, at first with Carol and finally on my own.
I was nervous about driving again, but Carol encouraged me to try. She drove me to a large, vacant, parking lot, and I slid into the driver’s seat. With trembling hands, I took the wheel and cautiously pressed the accelerator. Immediately I felt free again. It was like sprouting wings and being able to soar over the mountains and valleys.
I slowly drove around the parking lot a few times. “Do you think I could drive us home the back way?” Carol nodded yes, and I pulled out onto the road. It was a little scary, but I pressed down on the accelerator pedal and felt the car speeding up to the speed limit. I was a little wobbly at first, but after the first few minutes I was driving okay and we made it home safely.I was so thankful to be feeling better and doing things for myself again.
As the days continued to pass by, I realized that I was no means recovered yet. I still suffered from brain fog, and on some days I just couldn’t put things together quickly or accurately in my mind. For example, I would go to do something, and when I got to my destination I would completely forget what I was going to do. Or I would forget the names of people I had known all my life. And there were days when I would be very short of breath, gasping for air. Or days when I would just feel terrible as if hungover from drinking. My energy and stamina were still greatly reduced and any kind of sustained effort would quickly wear me out.
I had gone back to work at my office about three months after leaving the hospital. But I knew that I wasn’t able to do the job as well as before, so I decided to go ahead and retire.
On the very day of my retirement, my brother’s new apartment lease went into effect, and he moved back to Tennessee. My mother, whose dementia was worsening every day, moved back in with Carol and me. Though she was for the most part gentle and quiet, caring for mother proved to be challenging. She could never be left alone and, as her immediate recollection of people and things and short term memory continued to rapidly fade, we had to make significant changes to our schedule and lifestyle.
Mother was mistrustful of anyone not familiar staying with her. For this reason, and because of the risk of exposure to the coronavirus, Carol and I resigned ourselves to being mostly home bound. I had the opportunity to go back to work part time, mostly working from home. I was thankful and grateful to be able to do this. Carol, whose worked had suffered from the pandemic began to think of ways to bounce back, mostly working from home. My stepdaughter, Faith, who my mother is comfortable with, began working as a sitter one day a week so Carol and I could get away together for breaks.We slowly began to fall into a routine.

I began seeing doctors again, seeking help for the sleep disorder that was keeping me on supplemental oxygen at night. Something was still bad wrong with me, and most days I felt terrible. I had gained a lot of weight since getting out of the hospital and no amount of exercise or dieting seemed to allow me to lose it back off. It’s as if my entire system was out of whack.
I feared that my body was becoming dependent on the oxygen, so I called the medical equipment company and had them come and get the oxygen equipment.
Almost a year from the day the pulmonologist warned me that my O2 was going dangerously low when I was sleeping, a sleep disorder doctor, recommended by a friend, prescribed a CPAP.
Today, things are slowly getting better, but we are still fighting an uphill battle. We have had to learn how to be content with our circumstances and, at the same time, never stop striving and fighting to get back to normal. We have accepted that the goals and dreams we had before aren’t likely to be achieved the way we planned, but we will never give in to abandoning them; instead we will find alternate ways to get there.
We have changed, and so has the world. But we consider our change to be growth in all aspects of life.
Anyway, thanks for hanging in there. In part two I want to go inward and explore how the last two years affected me and Carol mentally, emotionally and spiritually. I’m thankful to be able to have written this much, as dull and lacking as it may be. I know that all of you have pandemic stories too, and I encourage you to share them with whoever God puts in front of you. The thing is, in spite of how different from each other we may think we are, we are much the same. Like snowflakes we all have differences, but are made of the same elements. Like snowflakes, we all have the same origin.

© 2021 by Larry and Carol Smith
Be strong and of good courage, and do it: fear not, nor be dismayed: for the Lord God, even my God, will be with thee; he will not fail thee, nor forsake thee, until thou hast finished all the work for the service of the house of the Lord (1 Chronicles 28:20).
